Healthcord Webinar Series
Stem cell capabilities
Duration
13:30 minutes
Category
Stem cell basics
Series
Stem cell capabilities
Objective
Educational
What you will learn
- Embryonic development and stem cell potential
- What are embryonic stem cells?
- The difference between adult and newborn stem cells
- Sources of hematopoietic stem cells and their differences
- How are embryonic stem cells obtained?
- What is stem cell potential?
- What are hematopoietic stem cells?
Stem cells and their capabilities
This webinar explores three types of stem cell being explored by researchers, their origins, and how stem cell source impacts their therapeutic capabilities.
To learn more about the origin of stem cells, we need to begin with human embryonic development. Life begins as a single fertilized egg. Following fertilization, this single cell undergoes many significant changes to produce a baby with more than 200 different types of cells in the body.
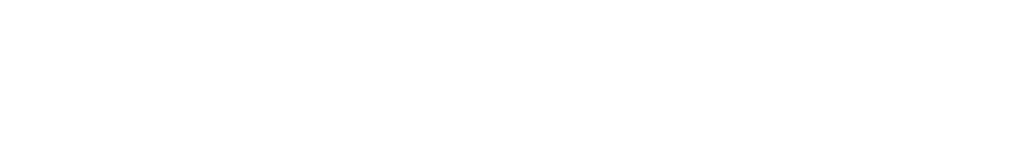
 All of the developmental stages highlighted here take place in the first week of pregnancy. The fertilized egg goes through several cell divisions to create the first structure of early development known as the blastocyst.
All of the developmental stages highlighted here take place in the first week of pregnancy. The fertilized egg goes through several cell divisions to create the first structure of early development known as the blastocyst.
If we focus on the stages before the formation of the blastocyst, these cells in the early embryo are identical.
They are undifferentiated, which means that they are not programmed to act or behave like any specialized cells in the body.
They are also totipotent, meaning that these cells can give rise to any type of cell in the body, or even produce an entire embryo.
Identical twins are a great example that highlights the capabilities of these early-stage cells. Monozygotic identical twins occur a single fertilized egg splits off during the early stages of development and give rise to two separate identical babies.
 Let’s go back to early development. The very first differentiation event occurs with the formation of the blastocyst.
Let’s go back to early development. The very first differentiation event occurs with the formation of the blastocyst.
The unorganized cells in the morula get reorganized to form the blastocyst, the hollow ball of cells. The first differentiation event in embryogenesis happens with the formation of the blastocyst.
Cells in the morula are identical and totipotent. They can give rise to any type of cell found in our bodies. The blastocyst consists of two types of cells, each with different capabilities.
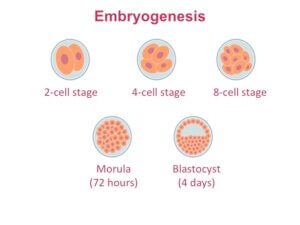
Here’s a closer view of the blastocyst. The layer of cells on the outside of the blastocyst is called the trophoblast.
These cells go on to make the placenta. The cells on the inside are referred to as the inner cell mass. They will give rise to the embryo or the baby.
These blue inner mass cells are pluripotent. They are capable of producing more than 200 different cell types found in the body. But they are more differentiated or specialized than the cells in earlier stages of development. Those early cells can make both the placenta and the embryo.
This brings us to the first type of stem cells, embryonic stem cells. Embryonic stem cells used in the lab are derived from the inner cell mass. Embryonic stem (ES) cells are highly controversial since they are derived from cells that have the capability to produce an embryo.
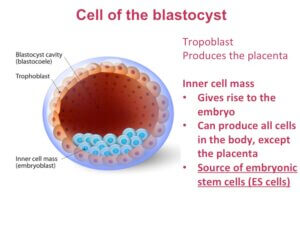
 How are embryonic stem cell lines generated? Before we discuss that, we need to understand what happens between fertilization and implantation.
How are embryonic stem cell lines generated? Before we discuss that, we need to understand what happens between fertilization and implantation.
Implantation is when the fertilized egg attaches to the wall of the uterus. Fertilization takes place in the oviduct, the tube that connects the ovary to the uterus.
All of the early cell divisions occur as the embryo travels down from the oviduct into the uterus. Implantation happens once the embryo reaches the blastocyst stage. This is why doctors can now use in vitro fertilization (IVF) to help with fertility.
During an IVF procedure, egg and sperm cells are mixed to allow fertilization to take place. Successful embryos are then cultured for a few days before some of them are transplanted into the mom.
In a majority of the cases, the remaining embryos are cryopreserved for later use. But in some cases, around 2.8% of IVF cases in the US, these embryos have to be discarded.
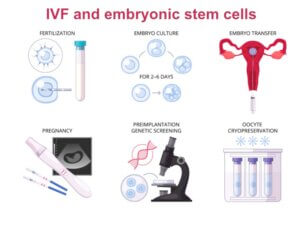 Human embryonic stem cells currently in use in the US were derived from such IVF embryos that would have otherwise been discarded. Given their origin, the inner cell mass, ES cells are pluripotent. They are able to self renew or continue to grow indefinitely.
Human embryonic stem cells currently in use in the US were derived from such IVF embryos that would have otherwise been discarded. Given their origin, the inner cell mass, ES cells are pluripotent. They are able to self renew or continue to grow indefinitely.
This is why ES cells are highly sought after for research involving cell therapy, transplantation therapy, and regenerative medicine. They are also being used for drug development and disease modeling.
But there’s one major limitation associated with ES cells. Using them for research purposes, let alone for cell therapy, remains highly controversial.
We will now return to early development, so the origins of the remaining stem cell types can be described.
When scientists talk about stem cells potential, they are refer to a stem cells ability to give rise to other types of cells. As you may remember, the very early cells of the embryo are totipotent. These cells can produce both the placenta and the embryo. The cells of a blastocyst are pluripotent, they can produce either the placenta or the embryo but not both. Stem cells with greater potential can give rise to more cell types.
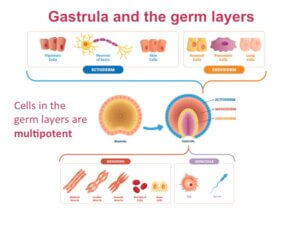 After implantation, the cells of the embryo become more and more specialized. In the next developmental stage, called the gastrula, cells within the blastocyst are reorganized into a multilayered structure.
After implantation, the cells of the embryo become more and more specialized. In the next developmental stage, called the gastrula, cells within the blastocyst are reorganized into a multilayered structure.
Cells of the gastrula are even more specialized the cells in the blastocyst. They are organized into three germ layers, which go on to produce specific cell types of the body.
These cells are multipotent, which means they are capable of producing several different types of cells but not all cell types.
Cells in the outermost layer or the ectoderm can produce skin cells, nerve cells and pigment cells. Cells in mesoderm or the middle layer produces muscle cells, bone cells and red blood cells.
The endoderm gives rise to pancreatic cells, cells that line our gut and lungs. And finally, the germ layer is responsible for making either egg or sperm cells.
This summary figure highlights how cell potency changes during development. Cells of the morula are totipotent cells, where each cell can produce an entire embryo and the placenta.
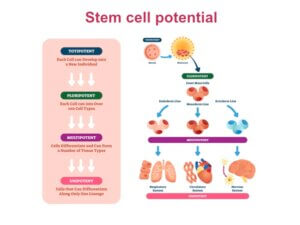 Next, they specialize in the blastocyst. Inner mass cells can produce all 200 types of cells in a human, but not the placenta. These cells are then further specialized when the germ layers are generated.
Next, they specialize in the blastocyst. Inner mass cells can produce all 200 types of cells in a human, but not the placenta. These cells are then further specialized when the germ layers are generated.
Multipotent cells of the germ layers can produce several different (but not all) cell and tissue types. At the opposite end are the unipotent stem cells. These cells differentiate along one type or lineage.
The two other types of stem cells described here, adult stem cells and newborn stem cells, are multipotent. They can give rise to many but not all different types of cells in the body.
All stem cells have the capability to self renew or keep producing more stem cells. This is a defining characteristic of stem cells. However, the potential of stem cells depends on their origin and age.
To date, researchers have discovered adult stem cells in a number of tissues. Adult stem cells are rare and very difficult to identify.What’s more, the exact origin of adult stem cells is still a mystery. Researchers can’t agree on whether they are “leftover” embryonic stem cells, or whether they arise in some other way.
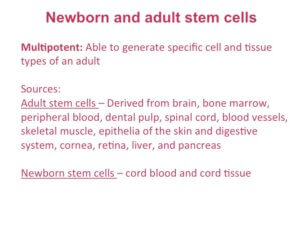 Cord blood and cord tissue are sources of newborn stem cells. The value of these stem cells in research and stem cell therapy is well established. Cord blood contains hematopoietic stem cells.
Cord blood and cord tissue are sources of newborn stem cells. The value of these stem cells in research and stem cell therapy is well established. Cord blood contains hematopoietic stem cells.
Hematopoietic stem cells were first identified more than 40 years ago. They are used extensively in stem cell transplants to treat many diseases.
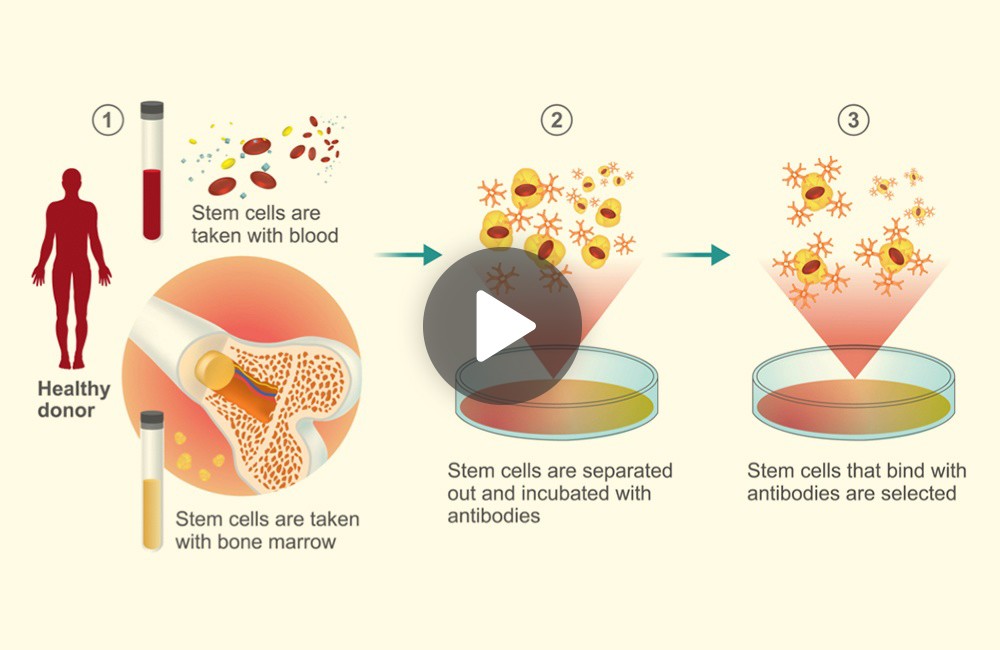
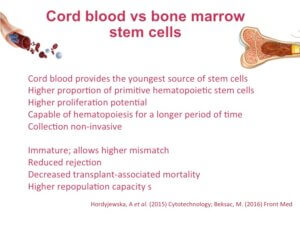
Hematopoietic stem cells are multipotent and they give rise to different types of blood cells and immune cells. They are found in both the bone marrow of an adult and in cord blood. But, stem cells taken from these two sources are not the same.
Stem cells from cord blood are at their youngest possible state, which means there is a higher proportion of primitive hematopoietic stem cells in cord blood. Studies show that stem cells from cord blood have higher proliferative potential (3-15 times that of bone marrow).
These young stem cells from cord blood have longer telomeres, which means they can undergo hematopoiesis (the process of making blood cells) for a longer period of time. When it comes to sample collection, taking samples from bone marrow involves surgery. Collecting cord blood is non-invasive and painless, but can only be performed after birth.
 Before a hematopoietic stem cell transplant is performed blood samples from the donor and the recipient are compared to see if they match. This is done by looking at markers on the surface of cells called HLA antigens.
Before a hematopoietic stem cell transplant is performed blood samples from the donor and the recipient are compared to see if they match. This is done by looking at markers on the surface of cells called HLA antigens.
Studies show that cord blood stem cells allow greater mismatching, meaning the match between the donor and the recipient does not have to be perfect. Researchers believe the immaturity or the primitive nature of stem cells in cord blood is behind this observation.
Other studies show that transplants involving cord blood stem cells associated with reduced rejection and reduced transplant-associated mortality rates.
Studies also show that cord blood stem cells have higher re-population capacity, or the ability to replenish the immune system, than stem cells from bone marrow.
Given the enhanced potential of cord blood stem cells, preserving them when possible with cord blood and cord tissue banking is recommended to all expectant parents.
Let’s look at the role of hematopoietic stem cells (HSCs) in a bit more detail. It was already mentioned that hematopoietic stem give rise to different types of blood cells and immune cells. Given that certain types of blood cells like our red blood cells have a very short life span, having the ability to replenish them is absolutely essential.
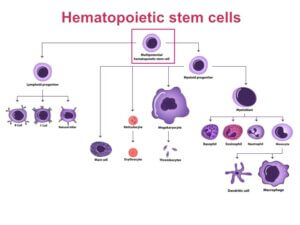 Replenishment of blood cells happens largely in the bone marrow. Typically stem cells produce intermediate cell types called progenitor cells that are not fully specialized. These cells then produce the more specialized cells that are necessary for function.
Replenishment of blood cells happens largely in the bone marrow. Typically stem cells produce intermediate cell types called progenitor cells that are not fully specialized. These cells then produce the more specialized cells that are necessary for function.
HSCs produce two types of progenitor cell types, lymphoid progenitors and myeloid progenitors.
Lymphoid progenitors regenerate the cells of the immune system. Myeloid progenitors are responsible for generating several different types of blood cells, including red blood cells.
Hematopoietic stem cells are likely the most extensively studied type of stem cells. They are already been used in clinical applications to restore blood cells and immune cells via bone marrow transplantations.
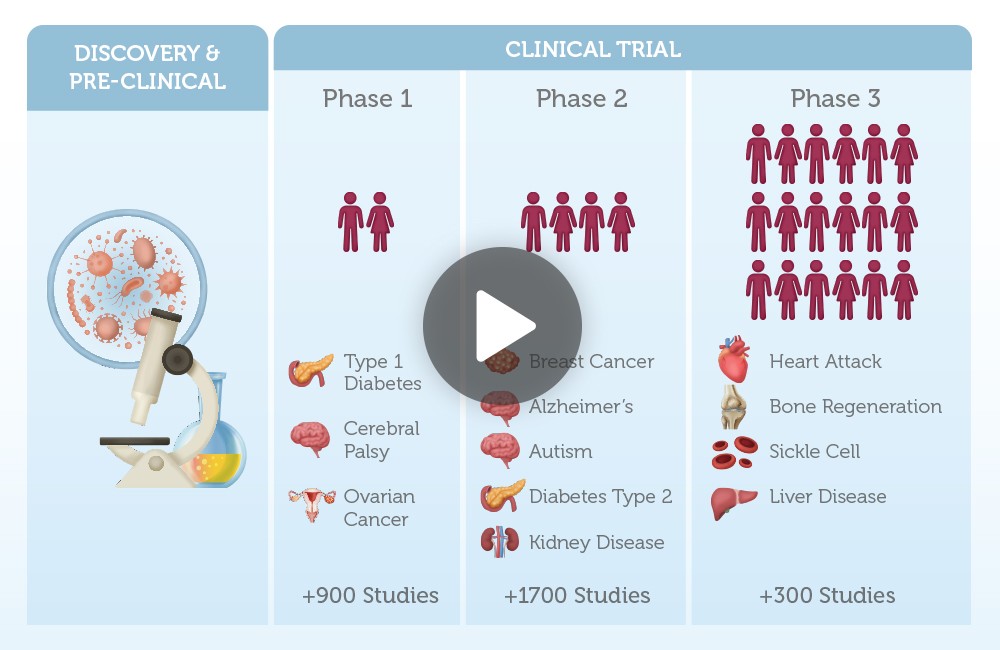
Around 80 different diseases are currently treated with hematopoietic stem cells from both bone marrow and cord blood. Hematopoietic stem cells were explored in detail as part of the cord blood basics seminar series. If you want to know more, we recommend checking out that webinar.
In summary, stem cells are defined by their ability to self renew and give rise to other types of cells in the body. But not all stem cells are made equal. Stem cell potential dictates the number and types of cells they are able to regenerate. Stem cells with higher potency are capable of producing more cell types than a cell with lower potency. Finally, we highlighted hematopoietic stem cells as an example of a multipotent stem cell currently in used for regenerating cells in the immune system and the blood system.
Both adult and newborn stem cells are being explored in clinical trials for their potential for treating a number of highly prevalent diseases such as diabetes, heart disease and Alzheimer’s.
More topics you might like
Continue your journey by selecting another topic.
What are newborn stem cells and why are they important?
3:45 minutes | Stem cell basics
Understand the different types of stem cell transplants.
5:30 minutes | Stem cell basics
Learn about the exciting new ways stem cells are being explored as a future therapeutic.
5 minutes | Stem cell basics
A Precious Gift of a Lifetime
Registering for stem cell banking takes only a few minutes.
A Precious Gift of a Lifetime
Registering for stem cell banking takes only a few minutes.